Whenever I scroll through any parenting group news feed, it’s not too long before I find yet another post from a mother asking about induction of labor. It’s neither unusual, nor surprising at this point because every year the rate of induction seems to be rising in this country! Often the reasons for the induction are because they have passed their due date. I’ve even heard stories of care providers inducing women ON their due date, just because nothing seemed to be “happening” to start labor.
A lot of times women ask how they can get into labor on their own, to avoid the induction. The responses given to this question show a pattern of thinking in our society that is troubling. There are many suggestions given on how to “induce” labor, and I can tell you right now that none of them actually work unless the baby was coming anyway! How do I know? Because I tried everything to get my stubborn little daughter to come early, and she would not have it! She was happy to put me through tons of prodromal labor, sure, but actually come out and end my torture? Nope! So, walking and climbing stairs? Been there! Eat spicy foods? Did that, got heartburn! Sex? I exhausted my husband with my demands! Nipple Stimulation? That was the only good use for the breast pump, and still didn’t work anyway! Red Raspberry Leaf Tea, contrary to popular belief, does not induce labor. I knew this, and so it was proven by the 2 cups of the stuff I drank each day from 36 weeks to the night before she was born! As for Evening Primrose Oil? You can stuff your vagina like a clown car and nothing is going to happen if your baby doesn’t want to vacate the premises! The only thing I didn’t try was Castor Oil, because every wise midwife I have spoken to has told me that Castor Oil is a BAD TIME and not at all a good idea for a pleasant labor. My point is that babies are not so easily evicted. That being said, I understand why so many women ask that question!
If you ask this question, you might be led to believe that induction “isn’t that bad” by moms who chose induction for themselves but they have no framework to compare between induced labor and true physiological birth. Some women state that they would rather induce than go another day being pregnant, but aren’t aware of the benefits to themselves and their babies of waiting for labor to start on its own. Some even believe (falsely) that if they don’t go into labor by 40 weeks they never will. I have seen the phrase “I don’t go into labor on my own, so I have to induce” too many times to count, and each time it hurts my heart.
This doesn’t mean that it doesn’t have its place! I recognize that Induction of Labor is sometimes necessary for medical reasons, however most inductions occurring in hospitals today are not medically indicated. Unfortunately a lot of first time mothers are unaware of their rights to refuse induction, and more problematically, they are often not informed of the risks that induction can pose to them and their babies. The culture of convenience we reside in makes it seem like induction is more commonplace and normal than it should be, and women are choosing this option thinking that an induced labor is no different than letting a baby come when they’re ready.
The sad truth is that too many care providers will perpetuate this belief, citing everything from a baby growing “too big” to a failed placenta as a reason to induce labor on or before 40 weeks. As a result there are often policies around inducing labor simply because a woman has passed her due date or is getting close to her due date without any indications that labor will start soon, even though this is NOT Evidence Based.
There have been several articles published by medical professionals who do believe in evidence-based care, and statements on the subject of unnecessary induction are available from every governing body of Obstetricians, Midwives, and Gynecologists, such as The American College of Obstetricians and Gynecologists (ACOG), The World Health Organization (WHO), The College of Midwives, The Royal College of Obstetricians and Gynecologists (RCOG), The National Institute for Health and Care Excellence (NICE), The Society of Obstetricians and Gynecologists of Canada (SOGC) etc. Sadly, not everyone knows of these guidelines, and the more “common” induction becomes the more often a woman will think she “has to” induce or “should” induce.
Your Baby Isn’t Ready
For a long time, no one knew just how labor was triggered or why, but studies have since been done and evidence has come to light that it’s not OUR bodies that trigger labor, but our BABIES. Scientists recently discovered that there’s a protein that develops in the lungs of fully mature babies that acts as an irritant inside the uterus and triggers your body to secrete the hormones to begin contractions. This means that if you force the baby out before that protein has developed, then their lungs are not fully developed and ready for life outside the womb.
When induction is necessary for medical reasons the baby will likely need more medical attention at birth anyway, but unnecessary induction could mean that the baby might require medical attention that could otherwise have been avoidable. There could be issues with breathing, due to the fact that the protein in the lungs (called surfactant) never developed due to an early birth. The baby could be much smaller than originally thought, which might result in a low-birth weight baby. Finally, there could be issues with breastfeeding to consider. Dr. Rachel Reed and Katie James shared on a podcast that if the baby is not ready to begin life outside the womb, they may have difficulty latching onto the breast and may lag in the development of instinctual feeding behaviours that would lead to successful long-term breastfeeding. There is a lot that is still unknown about the long-term consequences of induction on babies. In the absence of complications where the risks of an early birth are outweighed by the risks of continuing the pregnancy, it’s best to err on the side of caution and let the baby pick their birthday. Like fruit on a tree, not all babies are ready at the same time. Some need more time to “ripen” than others.
Your Body Isn’t Ready
One thing I often ask women who are facing induction is whether or not they know their Bishop Score. The most common response I get is, “what’s that?”
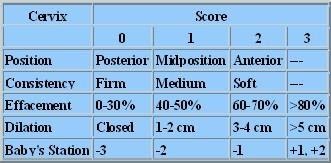
A Bishop Score is the number given based on how likely an induction will work for you, and it is CRUCIAL knowledge. Sadly a lot of clients go into their OB, doctor says “oh, you’re not going into labor anytime soon” and this leads them into thinking they need to be induced. The problem with this, aside from the fact that it’s not evidence based, is that a low Bishop Score (which is the likelihood that labor will start soon) has been linked with higher rates of c-section as the result of inductions that have “failed”. If your Bishop Score is low, then that means your body isn’t ready for labor to start yet, and forcing it to do something it’s not ready to do is going to cause it to take longer and likely lead to complications.
Your Labor Will Be Harder
I have friends and past clients who have experienced both physiological birth and induced birth, and the majority tell me that the experience was vastly different! They said they didn’t realize how far into labor they were with their non-induced births, because the contractions were so much milder and not on top of each other. After having both an induction and a physiological birth, they told me that they would never want to induce again unless absolutely necessary for their health or that of their baby.
Induced contractions are not the same as those that are brought on naturally; this is a proven fact. You aren’t getting the naturally occurring hormones in your body during an induction, which means that you also aren’t getting the endorphins necessary to help you cope with labor. The contractions will be longer, stronger, and closer together. Some women have reported that they had contractions one on top of the other, which is hard on your body AND on your baby. If the baby is in a bad position, this can lead to them getting “stuck” (called dystocia) because without that break between contractions it’s difficult for the baby to turn as needed. The force of being squeezed continuously could prematurely rupture the membranes (if they haven’t already broken your waters) which takes away that cushion in your uterus and on your cervix. Overall this leads to more pain and less ability to move around to cope; especially since you’re likely to have additional monitoring.
You Aren’t JUST Consenting to Induction
Induced labors require use of an IV, Continuous Electronic Fetal Monitoring (CEFM), and your labor is now being placed on a strict timeline to minimize fetal distress. An IV and the CEFM both restrict movement, which in turn makes it difficult to change positions and help the baby navigate through the pelvis. While it isn’t impossible to birth with an IV and the fetal monitoring, it does pose more difficulty in getting into effective birthing positions and increases the likelihood that you’ll need an assisted delivery or a c-section. I mentioned earlier that induced labor is more painful, but because you will not be able to produce your own endorphins it will most likely lead you to need an epidural to relax.
The epidural carries its own set of risks and while it can be helpful, it does have some disadvantages and potential side effects; even long-lasting consequences such as back pain at the injection site have been reported. The chances of this happening are small, but like everything the risks and benefits need to be evaluated by each individual and their circumstances. Back pain may not be a big deal for one woman but for someone who already has issues with their back and spine it could make their condition more severe. Finally, some hospitals require mothers who are induced to stay in bed, which likely would mean you would have a urinary catheter, which aside from not being very comfortable can also add the risk of contracting a urinary tract infection. This is just a few of the many possible interventions that may occur in an induced labor. The reality is that when you mess with the physiology of birth, it often leads to other complications that need to then be managed.
Pitocin is NOT Oxytocin
“The Drip”, “Oxytocin”, “Syntocinon” and “Pitocin” are the same drug by different names, depending on which care provider is using the terms. The most common and problematic term used for Pitocin is “oxytocin”, however, because people often confuse it with the hormone naturally produced during labor and assume there isn’t much difference between them. This couldn’t be further from the truth! Oxytocin produced by your body in labor crosses the blood-brain barrier and allows for the natural endorphins and feelings of relaxation and love to build up in your bloodstream, culminating with the birth of the baby. Nature designed birth this way specifically so that upon the birth of the baby the mothers would experience a birth “high” that aids in bonding and responsiveness to the newborn. The oxytocin your body produces also aids in breastfeeding. The contractions produced by Pitocin do not have these benefits to the mother and newborn as the drug cannot cross the blood brain barrier. Your body is also not producing its own oxytocin and endorphins, which means that you will not have the same ability to relax through contractions as in a physiological labor and there is no feedback from the uterus and the baby to your brain to tell it to either increase or decrease the levels of oxytocin and endorphins as needed. Without the bio-feedback, the contractions could be much stronger than what the baby can handle.
The Induction Could “Fail”
Note how I said the INDUCTION could fail, not your body. If your baby isn’t ready, then your body is likely to resist going into full-blown labor and induction could take much longer than if you were already going into labor on your own in a day or two. Depending on the method used, if the induction doesn’t work you could either be sent home, they’ll try a different method, or you’ll have a c-section. The use of the Prostaglandin “Cervadil” is the easiest induction method to walk away from if your body and baby are not ready; it’s inserted like a tampon and you can remove it yourself if the contractions are too strong or if nothing is happening, and your body could recover. Some care providers use a gel instead of the pessary method, however, and if this is the case then there is no way to remove the gel from inside your vagina and cervix. If you’re dilated “enough” then the next step is Pitocin, which is given through an IV and can be turned down or off once labor is established. Pitocin, as I already mentioned, is harder on your body and can cause fetal distress. The best case scenario with Pitocin is that when it’s turned off the baby recovers and you can try again in a few days or wait for labor to start on its own, however I’ve heard fewer cases of care providers actually sending mothers home if labor was well established before it was turned down/off. More likely the dosage will be turned up, or they won’t turn it off at all, and you will end up having a c-section for “failure to progress”, as this is a common reason given for doing a c-section.
If You’re a First Time Mother, Your Chances of a C-Section Are Higher
It has been noted since 1995 that induction of labor in a first time mother increases her chances of having a c-section. Currently in BC, 1 in 3 women will undergo a primary c-section with many of these having been induced labours for a “post dates” pregnancy. A primary c-section carries its own set of risks and if you’re planning on having more than one child then it is crucial that you weigh the risks that this could carry for future pregnancies. Fewer care providers are offering women the choice of a vaginal birth after more than one c-section, and fewer care providers even present a vaginal birth (VBAC) after ONE cesarean as a real choice for women. If a c-section becomes unavoidable, you will automatically have a more difficult task of finding a VBAC supportive care provider should you wish to have more children in the future. This isn’t to say that it can’t be done, but that is sadly the reality in our country for women seeking a VBAC. In some circumstances a c-section can be a life-saving procedure; however the World Health Organization has come out every year with the statement that the overall c-section rate should be around 10-15% for low-risk women. This means that over 15% of the c-sections being done in our hospitals could likely have been avoidable. As the induction rate continues to rise each year, and even each quarter, our c-section rates have risen as well.
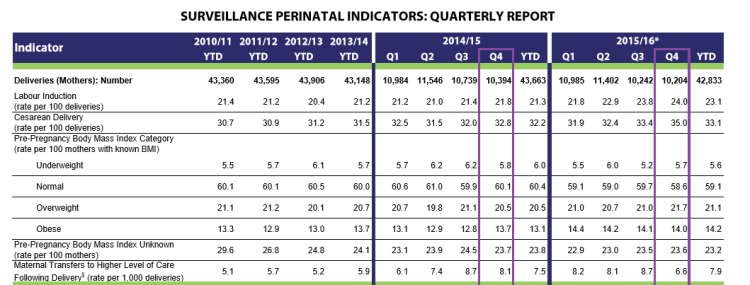
This image was taken from Perinatal Services BC website
As you can see, the rate of labor induction rises even when there are less deliveries in each quarter. For instance, Q4 of 2014/15 there were 10,394 deliveries and 21.8% of mothers were induced while 32.8% of all deliveries were c-sections. The following 2015/16 year in Q4 there were LESS deliveries with only 10, 204 women and a HIGHER induction rate of 24%. The c-section rate also rose to 35% in that final quarter. So we have less women giving birth, but MORE women undergoing induction and more women having c-sections in 2015/16 than the previous year. Finally, if we compare the induction and c-section rate to previous years the trend toward more inductions and resulting c-sections is quite concerning.
If you are trying to avoid a c-section, the best thing to do aside from choosing the right provider is to avoid induction unless medically indicated.
You Aren’t “Overdue” Until AFTER 42 Weeks
I feel that one of the greatest lies told to women is their “due date”, and that it does an even greater disservice to them. The last few weeks of pregnancy are hard and uncomfortable. You’re DONE! You are tired, sore, and just want to meet your baby. There isn’t a single woman who has gone over 40 weeks who DOESN’T understand this and there are a lot of women who have gone 41 weeks and beyond who know all too well how tempting that induction sounds. But the truth is that fewer than 5% of women ACTUALLY go into labor on their due date! A few will go into labor before then, but the average gestation for a first time mother is 41 weeks and 3 days. This means that there are women on BOTH sides of this average who are going into labor earlier or later. MOST women will go into labor by 42 weeks, almost all will have their baby by 43 weeks, and only a very tiny percentage of women will go into labor at 44 and 45 weeks depending on their menstrual cycles and other factors. So if you’ve reached or are approaching 40 weeks and nothing seems to be happening, the chances are very high that you’ll go into labor by 42 weeks on your own without having to do anything. If you reach 41 weeks gestation you can choose to go for monitoring every few days to check up on your baby and if there are still no medical concerns that would indicate the need for induction, then there’s no harm in waiting a few more days to see if labor will start on its own.
Your Baby Probably Isn’t THAT Big
If I had a nickel for every time I heard a mother say that she has to induce because the baby could get “too big” (called fetal macrosomia), I could probably afford to buy a birth house or twenty and set them up all over the Lower Mainland! The fact is that a late-term ultrasound is grossly inaccurate at being able to predict the size of the baby and after the first 14 weeks babies start to grow at different rates. That’s why not all babies are born at 40 weeks or even 41 weeks! Some grow faster, some need more time to catch up. I know women who gave birth at 41 weeks to 8 lb babies (mine was 7 lbs 13 oz) while their friends went a little past 41 weeks or even 42 weeks and had 6 lb babies! Also, something to keep in mind is that the skeleton is fully formed by the end of the second trimester and in the final month all the baby is gaining is FAT. Fat is squishy and adds mere ounces to the overall weight and size of the newborn, so even if you have your baby at 42 weeks there’s a slim chance that the weight would be much different if you induced a week earlier. The SOGC also advises AGAINST induction for fetal macrosomia if that’s the ONLY concern.
You Probably WILL Make It To The Hospital (And Even If You Don’t, It Doesn’t Have To Be a Disaster)
Sometimes women will induce because they fear they won’t make it in time/won’t know they’re in labor until it’s “too late”. The sensational stories of women giving birth in public places or in cars or being stuck at home are so common these days on social media that we often forget that these cases are the exception in birth, not the rule. If you’ve never given birth before, you are more likely to have a LONG labor (not necessarily painful, though) and will get to the hospital or other birthing location in plenty of time. HOWEVER, even if you turn out to be one of those women who “go fast” that doesn’t have to be scary. I believe that being prepared for anything is the best way to empower mothers in their births, and you should know that it is entirely possible to birth unassisted without ever needing to check dilation or time your contractions. I encourage you to read The Power of Pleasurable Childbirth and other books on physiological and unassisted birth even if your plan is to go to the hospital and have an epidural after the first contraction has started. This is because birth is unpredictable and sometimes contractions aren’t that strong, maybe not even that painful, and still result in a birth happening within 10 minutes without you even realizing it. If you realize that your birth is happening much faster than you thought, and you panic, that can make the situation more traumatic or even dangerous. If you’ve prepared your mind for this possibility then you’re able to remain calm and recall that information on what you need to do, and you have a greater likelihood of having a straightforward, safe birth in the car or in your living room. Finally, that fast, physiological birth that you didn’t anticipate might not be as painful as a similarly fast induced labor in the hospital.
Bottom Line: I’m not here to tell you what to do. If you still feel that induction is the right choice for you and your baby, then it is right. If, however, you feel pressured into induction, I wish to remind you that you are the sole decision maker in your care. Policies and Routine Standard of Care are NOT more important than your own individual feelings regarding induction. If you feel that you are being offered an induction without having any complications, then this information might give you some reassurance that you are “safe” to decline the induction and wait for labor to start on its own. You don’t “have to” induce if you don’t want to. You don’t “have to” try to get yourself into labor before a looming induction date to avoid it. You can say NO.
Were YOU pressured into induction by a care provider? How did you handle it? Let me know in the comments below!